The SMOC1 gene could be the key to stopping type 2 diabetes at its source.
Diabetes is a metabolic disease in which blood glucose levels remain elevated due to abnormal insulin function. In type 1 diabetes, the body does not produce this hormone; in type 2 diabetes (T2D), the body does not use it effectively. In Spain alone, 13% of the adult population lives with diabetes, a figure that continues to grow, driven by sedentary lifestyles, poor diet, and obesity.
Now, a scientific breakthrough provides a key piece of the puzzle. An international team of researchers has identified a gene called SMOC1, which plays a fundamental role in the development of type 2 diabetes. The study, published in the journal Nature Communications, explains why the beta cells of the pancreas—responsible for producing insulin—lose their function as the disease progresses.
When the pancreas “gets confused”: the origin of the problem
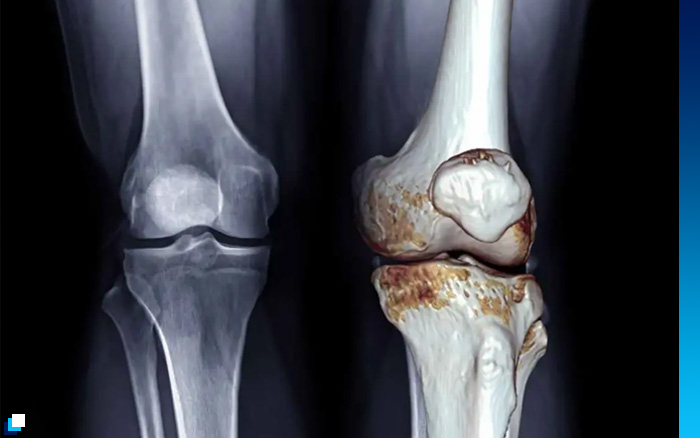
Inside the pancreas are the pancreatic islets, groups of cells that regulate blood sugar. There, two main players exist:
- Beta cells: produce insulin and decrease blood glucose
- Alpha cells: produce glucagon and increase blood glucose
Maintaining the balance between the two is essential for stable glucose levels.
The study reveals that in type 2 diabetes something surprising happens: some beta cells “forget” their original function, stop producing insulin, and begin to behave like alpha cells, generating glucagon. The result is devastating: less insulin, more blood glucose, and greater metabolic imbalance.
The role of the SMOC1 gene
To understand this “cellular identity crisis,” scientists analyzed pancreatic islets from 26 people (with and without diabetes) using advanced RNA sequencing techniques. This allowed them to classify five different types of cells and observe the progressive transformation from one into another.

The results pointed to a clear protagonist: the SMOC1 gene.
- In healthy individuals, SMOC1 is only active in alpha cells
- In people with type 2 diabetes, it begins to appear in beta cells, where it should not be
When SMOC1 is activated in the wrong place:
– insulin production is reduced
– the genetic identity of the beta cell is blocked
– the cell begins to produce glucagon
– blood glucose levels rise
Researchers even identified a third hybrid cell type, which they called “AB cells”, capable of producing both insulin and glucagon, confirming the ability for “role switching” within the pancreatic islet.

A new therapeutic target for type 2 diabetes
Until now, most treatments for T2D have focused on:
- Increasing insulin production
- Improving tissue sensitivity
- Reducing circulating glucose
But this research opens up a completely different approach: preventing beta cells from losing their identity and protecting their original function, by blocking or regulating the expression of the SMOC1 gene.
The next steps for the scientific team will be:
– Deciphering what activates SMOC1 in diabetic beta cells
– Understanding how its expression is regulated
– Developing drugs that block or modulate its activity
If successful, we could be looking at treatments capable of preserving beta cells and slowing disease progression, something no current drug fully achieves.
Conclusion
The discovery of the role of the SMOC1 gene offers a new explanation for the progressive deterioration of the pancreas in type 2 diabetes and points to a novel therapeutic target. This finding not only improves our understanding of the disease but also opens the possibility of future treatments that act at the cellular origin of the problem—not just its consequences.